
Many of us don’t think twice about chucking that economy-sized bottle of ibuprofen into our shopping carts right along with a head of lettuce and a jug of protein powder. Indeed, “Vitamin I” has become a staple strategy for reducing America’s pain and inflammation. Headache? Menstrual cramp? Backache? Overzealous-workout-induced muscle aches? Sure, ibuprofen can ease your discomfort. And I shouldn’t be picking on ibuprofen here—there are a plethora of other, so-called NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) out there. Drugs like aspirin, naproxen, and prescription-only agents like meloxicam and celecoxib (aka Celebrex) are quite fashionable as well.
Here’s a crazy stat for your next cocktail party (or not): each year, we Americans collectively pop a whoppin’ 30 BILLION doses of NSAIDs like ibuprofen and naproxen. I don’t think Costco makes a bottle THAT big….yet.
As a pharmacist, I don’t think there’s too much harm in the occasional use of drugs like ibuprofen or naproxen by people who have a healthy heart and blood pressure, good kidney and liver function, and a fortified gastrointestinal tract. But, I see that many people aren’t aware of the risks of frequent or chronic use of even over-the-counter (OTC) NSAIDs like ibuprofen and naproxen (aka Advil, Motrin, Aleve).
Let me break it down for ya:
- Roughly 1 of every 4 people who chronically use NSAIDs will develop an ulcer
- Risk of a gastrointestinal bleed or perforation (YIKES!) is about 4 times higher in people who use NSAIDs compared to those who don’t
- NSAIDs reduce blood flow to the kidneys and can result in kidney damage—especially if used frequently by people with high blood pressure, heart failure, or diabetes.
- About 1 in every 10 cases of drug-induced liver damage is due to NSAIDs
- If you take low-dose aspirin for cardiovascular health, some NSAIDs actually reduce the heart benefit of that aspirin
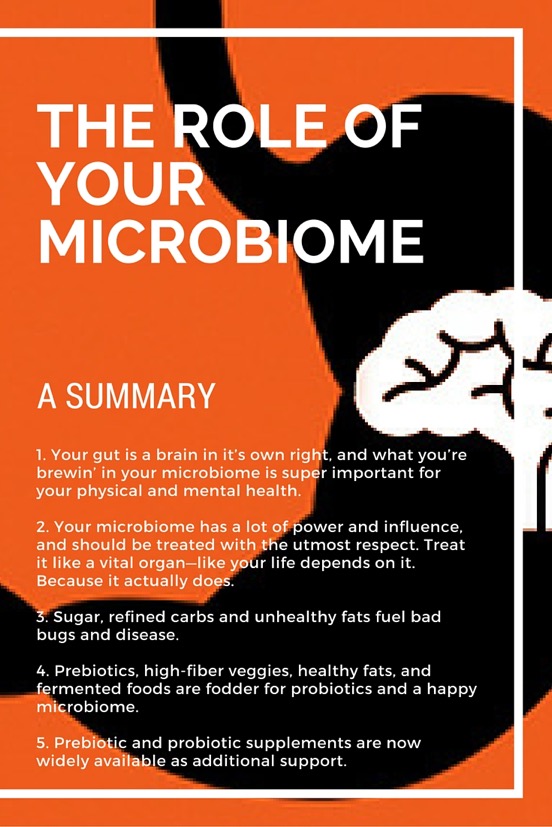
Back to the gut for a sec: scientists who want to better understand how NSAIDs (like OTC ibuprofen, naproxen, and regular-strength aspirin) cause ulcers have actually shown that they profoundly change the composition of the gut microbiome, and not for the better (if you missed my last post that espoused the magic of the microbiome, you can read it here). In other words, when we take NSAIDs, we are risking hostile takeover of our gut microbiomes by not-so-friendly bugs. And that could negatively affect our physical, mental, and emotional health as outlined in my previous post.
For all of the fitness enthusiasts out there, how often do you turn to OTC or prescription NSAIDs to ease joint or muscle aches? I’m hearing more and more that people in the athletic / fitness community are popping NSAIDs to keep injuries from “flaring up” or to reduce DOMS (delayed-onset muscle soreness) after workouts and training sessions. In addition to the stats on potential NSAID-induced adverse effects listed above, here’s another reason to pause before you pop that pill: researchers have shown (for decades) that NSAIDs actually impede the building and repair of muscle. And while the human data are more ambiguous than the dramatic effects seen in animal studies, the totality of evidence has convinced most experts to recommend against long-term use, especially of prescription doses of NSAIDs. The general consensus from a recently published review article in the journal Connective Tissue Research is that NSAIDs inhibit the healing process of connective tissue and the stimulating effect of exercise on connective tissue protein synthesis.
Interestingly, at least one study has shown that 400mg of ibuprofen (a standard OTC dose) had no more effect on post-exercise muscle soreness than placebo.
Healthy ways to quash inflammation
How can you continue your exercise / training routine while reducing the use of drugs like ibuprofen, naproxen, etc? What if you have chronic aches and pains?
Below I’ve included 5 non-NSAID strategies that can help reduce the amount of inflammation in the body and shift you back toward a healthy balance of inflammation. Remember that inflammation isn’t all bad! When we’re injured or have an infection, for examples, inflammation is crucial to the healing process—it’s how the body fights back and repairs damage. BUT, it’s important to consider that inflammation is not necessarily just an acute response to injury. More and more, researchers across multiple specialties—from the brain to the heart to the liver to the gut—are all finding that “silent”, chronic inflammation is a key underlying commonality of diseases like diabetes, heart disease, depression, ADHD, Alzheimer’s disease, liver disease and even cancer.
These 5 strategies below aren’t quick fixes—more like habits to be incorporated into your lifestyle.
- Cut down on sugar and processed food. Better yet, eliminate them. Sugar has been shown to trigger the release of chemical messengers in the body that promote inflammation. Processed foods in general ain’t doin’ you any favors.
- Choose fats that are rich in anti-inflammatory omega-3 fatty acids. Many food products in the aptly-acronymed SAD (standard American diet) are relatively heavy in pro-inflammatory omega-6 fatty acids. We do need omega-6 fatty acids, but the SAD tilts the scale waaaay to much in favor of omega-6—like about 20x too much! Many oils found in abundance in processed foods are high in omega-6, such as corn, peanut, vegetable, safflower and sunflower oils. And trans fats (hydrogenated oils) are also known to promote inflammation. In addition, grain-fed meats from factory farms are rich in omega-6. On the flip side, foods like avocados, olives, walnuts, almonds, flax seeds, chia seeds, pumpkin seeds, coconut, coconut oil & milk, grass-fed beef, pastured chicken (and eggs), grass-fed butter, and ghee (clarified butter) are all rich in omega-3 fatty acids.
- Get enough good sleep. Sleep is when our bodies repair. And the vast majority of us are not getting enough restorative, uninterrupted sleep. The American Academy of Sleep Medicine recently stated that sleeping fewer than 7 hours per night is associated with weight gain, diabetes, depression, heart disease, impaired immune function, increased pain, and impaired performance—lots of the same issues that are related to too much inflammation.
- Consider supplementing with omega 3 fatty acids. I personally take a tablespoon daily of Barlean’s Ultra High Potency Omega Swirl. It tastes great (my uber-picky 4-year old thinks it’s a treat to get a teaspoon after dinner), with NO burping / indigestion issues that people often complain about with capsules. By the way, one of the main reasons those fish capsules may be giving you the burps is because the oil is rancid. YUCK is right. To avoid this, be picky when buying fish oil—get one that is “molecularly distilled” which means that the oil has been purified enough to remove contaminants that promote rancidity. (Note that Barlean’s Omega Swirl does not say “molecularly distilled” on the bottle, but I checked the company’s website FAQ’s and their fish oils are ultra-purified through molecular distillation). Also, choose a fish oil with roughly 1000mg EPA and 500mg DHA (2 key types of omega-3)—don’t just look at the total milligrams of omega 3’s.
- If you have joint pain or other inflammation-related conditions, consider taking curcumin. This is a key component of turmeric, the yellow spice that gives curry its bright color! This substance has been studied for MANY types of inflammatory conditions ranging from diabetes to dementia, and is currently the subject of much ongoing research. Here are some VERY important considerations before you start taking a curcumin (or turmeric) supplement:
- Not a good idea to start curcumin if you are currently taking warfarin (Coumadin) or clopidogrel (Plavix). Curcumin can increase the anti-clotting effects of these drugs.
- Pick a supplement that contains a specific type of curcumin known as “BCM-95”. This specific formulation is much better absorbed. Turmeric capsules are very poorly absorbed, meaning that very little of it will actually get into your system. Several companies now make BCM-95 formulations. I have no ties / relationships with any of them. I personally take a brand called CuraMed (made by Terry Naturally), one 750mg capsule daily, and have had none of the GI distress that has been reported with other turmeric supplements.
My short take on all this:
There’s A LOT we can do to tamper inflammation that doesn’t involve medications that come with potentially counterproductive or even dangerous side effects. What we choose to do on a daily basis has a ginornmous impact on our levels of disease markers, including inflammation—both the kind that we feel as pain and the “silent” inflammation now recognized as a component of many chronic diseases. Our food choices, physical activity, and sleep are so important to our health. You may hear this advice all the time, but are you really checking into gauge your food, movement, and sleep habits? And if they aren’t so healthful, are you ready to make changes for the better?
Please share any questions you have about inflammation and treatment options, and I will do my best to provide answers!
Sources:
Lanza FL, Chan FKL, Quigley EMM, et al. Prevention of NSAID-related ulcer complications. Am J Gastroenterol 2009; 104:728–738. http://gi.org/guideline/prevention-of-nsaid-related-ulcer-complications/
Dideriksen K. Muscle and tendon connective tissue adaptation to unloading, exercise and NSAID. Connect Tissue Res. 2014;55:61-70.
Krentz JR, Quest B, Farthling JP, Quest DW, Chilibeck PD. The effects of ibuprofen on muscle hypertrophy, strength, and soreness during resistance training. Appl Physiol Nutr Metab. 2008;33:470-475.
Rutters F, Nieuwenhuizen AG, Lemmens SG, Born JM, Westerterp-Plantenga MS. Acute stress-related changes in eating in the absence of hunger. Obesity (Silver Spring). 2009;17:72-77. http://www.chicagotribune.com/lifestyles/health/sc-hlth-1118-dementia-sleep-20151112-story.html
 RENTALS
RENTALS ACTIVITIES
ACTIVITIES Menu
Menu ABOUT
ABOUT CONTACT
CONTACT